Understanding Pain and Discomfort of Toe Arthritis

Arthritis in the toe, a common ailment affecting many individuals, manifests through various symptoms that can significantly impact daily life. Persistent toe pain, particularly during movement or weight-bearing activities, are hallmark symptoms of toe arthritis. Individuals may experience stiffness and limited range of motion in the affected toe, making tasks like walking, bending, and standing challenging and painful. Swelling and inflammation surrounding the toe joint are also common symptoms of arthritis, indicating underlying joint damage and inflammation. As arthritis progresses, individuals may notice changes in the appearance and alignment of the toe, such as swelling, deformities, and bone spurs. Additionally, toe arthritis can cause instability and weakness in the affected joint, leading to difficulty bearing weight and maintaining balance. If you are experiencing toe pain, it is strongly suggested that you consult a podiatrist who can diagnose the cause, and offer appropriate relief and treatment options.
Toe pain can disrupt your daily activities. If you have any concerns, contact Renee Rodriquez, DPM of Foot Clinic of South Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toe Pain
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
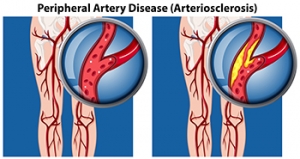
Walking and Peripheral Artery Disease

Peripheral artery disease, or PAD, can cause crampy, painful sensations in the legs during walking, often dismissed as mere exertion or aging. However, it is important not to overlook these symptoms, as PAD stems from fatty deposits that obstruct blood flow in the arteries outside the heart and brain. The lack of blood flow to the lower extremities can result in serious foot problems. Risk factors of peripheral artery disease include smoking, high cholesterol, high blood pressure, and diabetes. Classic PAD pain, known as claudication, typically occurs in the calf and subsides with rest. But other signs, like coldness, discoloration, or slow-healing sores in the feet may indicate inadequate blood supply, necessitating prompt treatment. Early detection via tests like the ankle-brachial index is vital, with lifestyle changes, such as quitting smoking, maintaining a healthy diet, and regular exercise, playing a key role in PAD management. Walking enhances blood flow in smaller leg arteries, creating alternative pathways to alleviate pain. Health experts recommend at least 30 minutes of walking, three times a week, for individuals with peripheral artery disease, to help slow the progression and associated complications. For help with the foot problems linked to PAD, it is suggested that you schedule an appointment with a podiatrist as quickly as possible.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Diagnosing a Lisfranc Fracture

Lisfranc fractures, occurring deep within the midfoot, present a diagnostic challenge due to their intricate location amidst a multitude of bones and tendons. Often misdiagnosed, these fractures result from either broken bones or torn ligaments supporting the midfoot structure. A Lisfranc fracture can range from mild muscle tears to complex fractures that involve multiple bones and joints. Lisfranc fractures are commonly mistaken for a simple foot sprain and can lead to prolonged pain and complications if left untreated. Low-energy incidents, like missteps or falls during routine activities, typically cause these fractures. High-energy traumas from elevated falls also can result in this type of injury. An accurate diagnosis of a Lisfranc fracture is challenging and requires a thorough evaluation by a podiatrist, using advanced imaging techniques. Proper treatment of Lisfranc fractures, ranging from conservative measures to surgical intervention, is essential for optimal recovery, as ignoring the injury or attempting to walk it off can worsen damage and prolong healing time. If you are experiencing severe pain in the midfoot area, it is suggested that you schedule an appointment with a podiatrist as quickly as possible for a complete exam and diagnosis.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
Causes of Bone Spurs on the Heel

Heel bone spurs, medically known as osteophytes, are abnormal growths that can result in pain and restricted movement. Often unnoticed until visible on an X-ray, heel bone spurs are associated with degenerative joint diseases, such as osteoarthritis, where the breakdown of joint cartilage prompts the body to form new bone as a reparative measure. This process leads to the development of bone spurs along the edges of affected joints, particularly in the heel region. Besides aging, various factors contribute to heel bone spurs, including injuries and overuse, common among runners and dancers. Other factors are hereditary predisposition, obesity, and congenital bone issues. Many people may have heel bone spurs without symptoms, but others can experience pain and loss of joint mobility if the spur rubs against bones or presses on a nerve. If you suspect you have a heel bone spur or are experiencing unexplained heel pain, it is suggested that you schedule an appointment with a podiatrist for a comprehensive evaluation and the appropriate treatment plan.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Brownsville, TX . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
A Comprehensive Approach Toward Preventing Running Injuries

Ensuring a safe and injury-free running experience involves adopting effective prevention techniques that prioritize the well-being of your muscles and joints. Start with a proper warm-up routine, incorporating dynamic stretches to prepare your body for the demands of running. Gradually increase the intensity and duration of your runs, allowing your muscles to adapt to the stress gradually. Invest in well-fitted running shoes that provide adequate support and cushioning, considering factors like arch type and pronation. Cross-training activities, such as strength training and flexibility exercises, play a critical role in enhancing overall muscle balance and resilience. Paying attention to your running form and maintaining a posture that minimizes impact on joints may help to reduce the risk of injury. Adequate rest and recovery are equally vital, and listening to your body allows it time to recuperate between runs. By adopting a holistic approach that encompasses warm-ups, proper gear, cross-training, form correction, and rest, you can significantly reduce the likelihood of running-related injuries and enjoy a sustained and fulfilling running journey. If you have sustained a foot or ankle injury from running, it is suggested that you speak to a podiatrist.
All runners should take extra precaution when trying to avoid injury. If you have any concerns about your feet, contact Renee Rodriquez, DPM of Foot Clinic of South Texas. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
There are a lot of mistakes a runner can make prior to a workout that can induce injury. A lot of athletes tend to overstretch before running, instead of saving those workouts for a post-run routine. Deep lunges and hand-to-toe hamstring pulls should be performed after a workout instead of during a warmup. Another common mistake is jumping into an intense routine before your body is physically prepared for it. You should try to ease your way into long-distance running instead of forcing yourself to rush into it.
More Tips for Preventing Injury
- Incorporate Strength Training into Workouts - This will help improve the body’s overall athleticism
- Improve and Maintain Your Flexibility – Stretching everyday will help improve overall performance
- “Warm Up” Before Running and “Cool Down” Afterward – A warm up of 5-10 minutes helps get rid of lactic acid in the muscles and prevents delayed muscle soreness
- Cross-Training is Crucial
- Wear Proper Running Shoes
- Have a Formal Gait Analysis – Poor biomechanics can easily cause injury
If you have any questions, please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.