Choosing the Right Running Shoe for Your Foot Type
Running may seem like a simple to do. However, running is actually a complex movement that puts stress on the ligaments, bones, and joints of the body. Selecting the correct running shoe is important for increasing performance and avoiding risk of injury. Running shoes should be selected based on your foot type. Considerations such as trail versus road shoes are important. Your foot type dictates the degree of cushioning, stability and motion control you require. The most accurate way to learn your foot type is to visit a local shop that specializes in running shoes. Professionals can measure your arch type, stride and gait and help you with your shoe needs.
The design of running shoes is created around the idea of pronation. Pronation is the natural rolling movement of your ankle from the outside to inside when your foot strikes the ground. If you run properly you strike the ground on the outside of your heel and roll in the direction of your big toe before pushing off once more. Pronation is beneficial because it assists the lower half of your body in absorbing shock and storing energy. Those considered neutral runners pronate correctly and do not need running shoes that help correct their form. Neutral runners can choose from a wide variety of shoes, including barefoot or minimal types. However, those who have arch problems or who adopt an incorrect form while running may experience too much or too little pronation. They may require running shoes that offer additional support.
Those who overpronate experience an over-abundance of ankle rolling. Even while standing, those who severely overpronate display ankles that are angled inward. It is not uncommon for them to have flat feet or curved legs. The tendency to overpronate may cause many injuries. Areas that tend to become injured are the knees, ankles, and Achilles tendon. If you find that you have a tendency to overpronate, you should look at shoes that provide extra stability and motion-control. Motion-control shoes are straight and firm. Shoes of this type do not curve at the tip. The restricted flexibility along the middle of the shoe prohibits the foot from rolling too far inward as your foot strikes the ground.
A less common problem is underpronation. Underpronation, also called supination, is when the feet are unable to roll inward during landing. Those who underpronate have feet that lack flexibility and high arches. This prevents any kind of shock absorption, even though it does place less rotational stress on ankles and knees. This added force can cause fractures, ligament tears, and muscle strains because the legs are trying to compensate for the impact. Those who underpronate need shoes with more cushioning and flexibility. If you have a tendency to underpronate, selecting stability or motion-control shoes may cause you more problems by continuing to prevent pronation.
Keeping Feet Healthy and Beautiful for Life

Feet carry us through every stage of life, yet they are often neglected until discomfort arises. Maintaining their appearance is not just about aesthetics. It is about care, comfort, and confidence. Just as a well-kept garden thrives, feet need regular attention to stay smooth, strong, and youthful. Hydration is key. Skin that is nourished with moisture resists cracks and roughness. Gentle exfoliation removes dull layers, revealing fresh, soft skin beneath. Strengthening exercises keep feet agile, preventing stiffness and imbalance that can lead to poor posture. Wearing properly fitted shoes preserves natural alignment, preventing issues that accelerate aging. Over time, nails can thicken or discolor, but trimming them correctly and keeping them clean prevents complications. Investing in foot care today means walking with ease tomorrow. If pain, calluses, or nail changes become a concern, it is suggested that you see a podiatrist to keep your feet looking and feeling their best.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Elderly Foot Care
As you grow older, you will start to notice more problems with your feet due to wear and tear. This may also happen because the skin will start to become thin and lose elasticity. Some signs of aging feet are regular aches and pains, bunion development, and clawed toes.
Fortunately, there are ways you can improve comfort, relieve pain, and maintain mobility in your feet. One of the best ways to deal with aging feet is to exercise. If you keep active, your muscles will become toned which will then strengthen the arches in the foot and stimulate blood circulation.
It is important that you practice proper foot care to protect your aging feet. You should wash your feet in warm water on an everyday basis. Afterward, the feet need to be dried well and it is important to dry between the toes. Your toenails should be trimmed and kept under control; nails that are poorly cut may become ingrown. At the end of each day, performing an inspection of your feet will allow you to detect any ailments in their early stages.
As you grow older, it becomes more important that you wear comfortable shoes. Your shoes should be secure, and they should provide decent arch support. If you are looking to buy a new pair of shoes, it is best to look for a pair that are made from a breathable material. It is also helpful to have shoes that have a bit of extra room at the top of the shoe, especially if you suffer from swollen feet.
The most common foot problems that elderly people will encounter are bunions, calluses, corns, hammertoes, heel pain, and foot problems related to diabetes. Some other issues include arch pain, tarsal tunnel syndrome, Achilles tendonitis, and Morton’s neuroma
An annual foot examination is a great way for you to ensure that you do not have any serious health problems with your feet. You should talk to a podiatrist about the available treatment options for whichever foot issue you are dealing with.
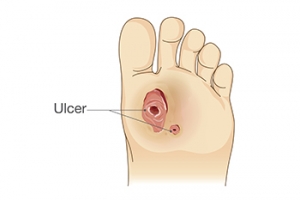
Pressure Sores Can Lead to Foot Ulcers
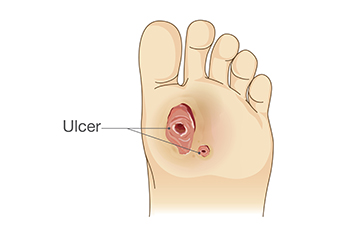
Rubbing points, also termed pressure sores, on the feet, toes, or ankles can progress into serious foot ulcers if left untreated. These pressure sores develop when prolonged pressure reduces blood flow, damaging the skin and underlying tissues. People with health conditions that impair circulation, such as diabetes or vascular disease, face a higher risk. Pressure sores are classified by severity, starting as red, painful skin and potentially worsening into deep wounds that expose muscle or bone. Common rubbing sites include the heels and bony areas of the foot. Without proper care, these wounds may become infected, further complicating healing. A podiatrist can assess the severity of a pressure sore and recommend appropriate treatment to prevent complications. This may involve wound care, pressure relief strategies, specialized dressings, or in severe cases, surgery to remove damaged tissue. Regular monitoring and professional treatment are essential to reduce the risk of infection and promote healing. If you have foot sores that are not healing properly, it is suggested that you schedule an appointment with a podiatrist for wound care treatment.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
2 Common Types of Heel Spurs

Heel spurs are bony growths that develop on the heel bone, often leading to pain and discomfort. The two most common types of heel spurs are the anterior heel spur, or heel spur syndrome, and the posterior heel spur. An anterior heel spur is located on the bottom of the heel and is typically associated with plantar fasciitis. This condition causes pain in the heel, especially with the first steps in the morning or after long periods of sitting. A posterior heel spur forms at the back of the heel, near the Achilles tendon. It is often caused by repeated stress or overuse of the tendon and can result in pain and swelling at the back of the heel. Both types of heel spurs can be caused by excessive pressure on the feet, poor footwear, or improper walking mechanics. If you have heel pain, it is suggested that you contact a podiatrist who can accurately diagnose it and provide treatment options.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Brownsville, TX . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Symptoms and Treatment of Bunions

Bunions, medically referred to as hallux valgus, occur when the joint at the base of the big toe begins to protrude, often causing discomfort or difficulty in wearing shoes. A bunion develops as the tip of the big toe leans toward the other toes, leading to a wider foot structure. Symptoms of bunions include pain in the affected joint, swelling, redness, or numbness in the toes. In severe cases, bunions may limit mobility or contribute to other deformities like hammertoes. Risk factors include genetic predisposition, rheumatoid arthritis, or structural issues like flat feet. Wearing improper footwear, such as high heels or narrow shoes, can worsen the problem. A podiatrist can diagnose and manage bunions by evaluating the foot's alignment and identifying the severity of the condition. This foot doctor may recommend custom orthotics, adjustments to footwear, or, in persistent cases, surgery to correct the deformity and alleviate symptoms. If you have problems with bunions, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment options.
If you are suffering from bunions, contact Renee Rodriquez, DPM of Foot Clinic of South Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.