Managing a Toe Infection

Toe infections can cause significant discomfort, especially for those who are on their feet regularly. Common symptoms of a toe infection include redness, swelling, pain, and oozing, sometimes accompanied by a foul odor or warmth surrounding the affected area. Toe infections may result from ingrown toenails, fungal conditions, injuries, or poor hygiene. For people with diabetes, even a minor toe infection can quickly become a serious issue, due to reduced blood flow and nerve damage, and can potentially lead to severe complications if left untreated. Wearing tight shoes, improperly trimmed toenails, or exposure to bacteria and fungus in damp environments are common triggers of toe infections. A podiatrist can diagnose the underlying cause of a toe infection and provide targeted treatment, such as prescribing antifungal or antibacterial medications, or performing procedures like partial nail removal for severe ingrown nails. If you have a toe infection, it is suggested that you promptly schedule an appointment with a podiatrist for an exam and treatment.
Toe pain can disrupt your daily activities. If you have any concerns, contact Renee Rodriquez, DPM of Foot Clinic of South Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toe Pain
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
Non-Injury Causes of Foot Pain

Foot pain can arise from a variety of non-injury causes unrelated to exercise or repetitive stress. Skin issues like calluses, corns, or warts can create discomfort, particularly when they develop on weight-bearing areas of the feet. Conditions like athlete’s foot or contact dermatitis may cause itching, redness, and peeling skin. Joint-related problems, such as bunions, hammertoes, or arthritis, can lead to pain, swelling, and limited mobility. Nerve-related conditions, including Morton's neuroma or tarsal tunnel syndrome, often cause burning, numbness, or tingling sensations in the toes or feet. Circulation problems, such as those associated with diabetes or peripheral arterial disease, can result in nerve damage and lead to numbness, burning, or a lack of sensation in the feet. Age-related changes, including thickened nails or foot spreading, can also contribute to discomfort. A podiatrist is well-equipped to evaluate and manage these non-injury foot pain conditions through diagnostic techniques and personalized treatment options. If you are experiencing foot pain, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment options.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Puncture Wounds on the Feet

Puncture wounds on the feet are injuries where sharp objects, like nails, glass, or thorns, penetrate the skin and underlying tissues. These wounds often occur while walking barefoot, especially in outdoor environments or construction areas. Individuals at higher risk include children playing outside, workers in hazardous conditions, or anyone wearing inadequate footwear. The sensation varies but often includes sharp, sudden pain at the time of injury, followed by soreness or throbbing. If debris remains embedded, discomfort may persist, and swelling or redness can develop. Without proper care, these wounds risk infection, as bacteria can enter deep tissue layers. If you have sustained a puncture wound on your foot, it is strongly suggested that you schedule an appointment with a podiatrist promptly. This foot doctor will assess for foreign objects, clean the wound thoroughly, and determine if antibiotics or a tetanus shot are needed.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
The Dangers of Wearing Worn Out Running Shoes

Wearing worn-out running shoes can lead to foot, toe, and ankle problems as a result of inadequate support and cushioning. Over time, the foam and tread in running shoes degrades, reducing their ability to absorb shock and stabilize the foot. This can increase pressure on the arches, contribute to overpronation or underpronation, and lead to conditions like arch pain or Achilles tendon discomfort. Signs of wear include new foot pain, flattened midsoles, or uneven tread patterns. For runners with flat feet or for those who overpronate, worn out shoes can aggravate these structural issues, increasing the risk of foot and other injuries. Experts suggest that active runners replace their shoes every 300 to 500 miles, or approximately every six months. A podiatrist can assess a runner’s foot alignment, gait, and running habits to help them choose appropriate footwear and reduce injury risks. If you are experiencing foot pain after running, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries. If you have any concerns about your feet, contact Renee Rodriquez, DPM of Foot Clinic of South Texas. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
Many common running injuries are caused by overuse and overtraining. When the back of the kneecap starts wearing out and starts causing pain in your knee, this is commonly referred to as runner’s knee. Runner’s knee is a decrease in strength in your quadriceps and can occur if you’re not wearing properly fitted or supporting shoes. To prevent runner’s knee, focusing on hip strengthening is a good idea, as well as strengthening your quads to keep the kneecaps aligned.
What Are Some Causes of Running Injuries?
- One cause of a common running injury is called iliotibial band syndrome.
- Plantar fasciitis is also another common injury.
- Stress fractures can occur from overtraining, lack of calcium, or even your running style.
Best Ways to Prevent Running Injuries
- Wear footwear that fits properly and suits your running needs.
- Running shoes are the only protective gear that runners have to safeguard them from injury.
- Make a training schedule. Adding strengthening exercises as well as regular stretching can help keep you strong and limber and can lessen the possibility of injuries.
- Stretching keeps muscles limber; this will help you gain better flexibility.
If you have any questions please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Prevent Running Injuries
Overtraining and overusing the feet are the main causes of common running injuries. A number of these common injuries are caused by overrunning. Runner’s knee is a condition that is characterized by the back of the kneecap beginning to wear away and cause pain in the knee. This frequently occurs due to either a decrease in strength in the quadriceps muscles or ill-fitting shoes that are lacking in proper support for the inside of the forefoot. Strengthening exercises focusing on the quad muscle and sports orthotics are the usual treatments for those suffering from runner’s knee. Prevention of the condition lies in a focus on hip strengthening and quad-strengthening to keep the kneecap aligned. To help learn the best exercise to heal runner’s knee, one can also undergo physical therapy.
One common injury, called iliotibial band syndrome, is often caused by overtraining. This condition occurs when the iliotibial band gets irritated, creating pain and discomfort in the outside knee area. Plantar fasciitis, another common running injury, also occurs as a result of inflammation and irritation. Plantar fasciitis is an inflammation and irritation of the bone in the foot. A large amount of pain is often experienced due to plantar fasciitis. The condition can be caused by a high arch, improper footwear, tight muscles, or flat feet. It can best be avoided by stretching and wearing appropriate footwear that supports the foot.
Another common injury for runners is stress fractures. These injuries occur due to running style, overtraining, or a lack of calcium. Stress fractures most often occur in several locations in runners, including the inner bone of the leg, the thighbone, the bone at the base of the spine and the bones of the toes. Stress fractures are best prevented by wearing proper footwear and by running on flat and hard surfaces; this will absorb some of the shock created during running.
Aside from overtraining, other causes of common running injuries include ill-fitting footwear, a lack of flexibility and strength, and irregular biomechanics. The best way to avoid running injuries is to prevent them from even occurring. Both iliotibial band syndrome and stress fractures are preventable. The first step that should be taken to prevent running injuries is to only wear footwear that fits properly and that is appropriate for whatever activity you are doing. Running shoes are the only protective gear available to runners that can safeguard them from sustaining injuries. Choosing the right pair of shoes is therefore extremely important. While running shoes are an important factor, it is also important to consider other facets of your running routine such as training schedules, flexibility, and strengthening. These elements should be considered and altered according to your running needs to best maximize your run and minimize the possibility of injury. Careful stretching before and after a run should also be considered to help prevent running injuries. Stretching muscles enables greater flexibility and a lesser chance of sustaining injury.
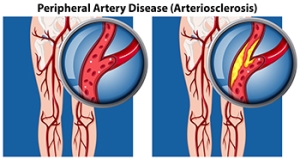
Facts About Peripheral Artery Disease
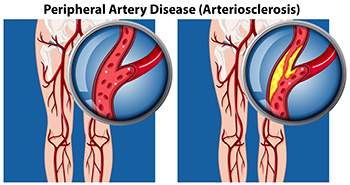
Peripheral artery disease, known as PAD, occurs when the blood vessels in the legs and feet become narrowed or blocked, reducing blood flow. This leads to symptoms like leg pain, cramping, or fatigue, particularly when walking or exercising. PAD can also cause sores or ulcers that are slow to heal, or cold, pale feet. In severe cases, it can increase the risk of infections or even amputation, if left untreated. The primary cause of PAD is atherosclerosis, a condition where fatty deposits build up in the arteries. Risk factors include smoking, diabetes, high blood pressure, and high cholesterol. Treatment for PAD often involves lifestyle changes, such as quitting smoking, exercising, and managing blood sugar and cholesterol levels. Medications or surgery may be necessary in more advanced cases. A podiatrist can assess your condition, provide effective treatments, and help prevent complications. If you are experiencing symptoms of PAD, it is suggested that you schedule an appointment with a podiatrist.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.