Symptoms of Plantar Fasciitis
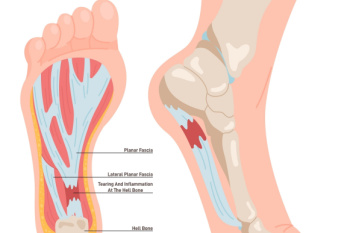
Plantar fasciitis can be a result of inflammation of the plantar fascia, which is the thick band of tissue connecting the heel to the toes. This condition typically occurs from repetitive strain or excessive pressure on the feet. It is commonly experienced by athletes, runners, and individuals who stand for extended periods. The hallmark symptom of plantar fasciitis is heel pain that is particularly sharp and stabbing, and often worsens with activity or after prolonged periods of rest. Additionally, individuals with plantar fasciitis may experience discomfort along the arch of the foot. While the severity of symptoms can vary, untreated plantar fasciitis can significantly impair mobility and quality of life. Early recognition and appropriate management, including rest, stretching exercises, orthotic devices, and in severe cases, surgical intervention, are important for effective relief and prevention of long-term complications. Plantar fasciitis is treated by a podiatrist. If you are experiencing any of the above symptoms, it is suggested that you contact this type of doctor who can successfully provide treatment.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Causes and Symptoms of Athlete’s Foot

Athlete’s foot, medically known as tinea pedis, is a fungal skin infection that can affect anyone regardless of their athletic pursuits. This highly contagious fungus spreads easily from person to person, and thrives in moist environments such as pools, locker rooms, and public showers. The fungus responsible commonly affects the feet, causing redness, itching, and skin flakiness between the toes. Other symptoms of athlete's foot include burning or stinging sensations, blisters, and thick or discolored toenails. Symptoms may differ, depending on the type of athlete’s foot infection. Toe web infection typically results in skin peeling and cracking between the fourth and fifth toes. Moccasin type infection presents as thick, cracked skin on the bottom of the foot, often near the heel. It is sometimes accompanied by a foul odor. Vesicular type infection leads to blisters on the sole of the foot. If you suspect you have athlete’s foot, it is suggested that you seek prompt treatment from a podiatrist to limit the spread of infection.
Athlete’s Foot
Athlete’s foot is often an uncomfortable condition to experience. Thankfully, podiatrists specialize in treating athlete’s foot and offer the best treatment options. If you have any questions about athlete’s foot, consult with Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor will assess your condition and provide you with quality treatment.
What Is Athlete’s Foot?
Tinea pedis, more commonly known as athlete’s foot, is a non-serious and common fungal infection of the foot. Athlete’s foot is contagious and can be contracted by touching someone who has it or infected surfaces. The most common places contaminated by it are public showers, locker rooms, and swimming pools. Once contracted, it grows on feet that are left inside moist, dark, and warm shoes and socks.
Prevention
The most effective ways to prevent athlete’s foot include:
- Thoroughly washing and drying feet
- Avoid going barefoot in locker rooms and public showers
- Using shower shoes in public showers
- Wearing socks that allow the feet to breathe
- Changing socks and shoes frequently if you sweat a lot
Symptoms
Athlete’s foot initially occurs as a rash between the toes. However, if left undiagnosed, it can spread to the sides and bottom of the feet, toenails, and if touched by hand, the hands themselves. Symptoms include:
- Redness
- Burning
- Itching
- Scaly and peeling skin
Diagnosis and Treatment
Diagnosis is quick and easy. Skin samples will be taken and either viewed under a microscope or sent to a lab for testing. Sometimes, a podiatrist can diagnose it based on simply looking at it. Once confirmed, treatment options include oral and topical antifungal medications.
If you have any questions, please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Deal with Athlete's Foot
Athlete’s foot is a type of fungal infection that affects the skin on the feet. It is caused when the tinea fungus grows on the foot. It is possible to catch the fungus through direct contact with someone who has it or by touching a surface that is contaminated with it. This type of fungus thrives in warm, moist environments such as showers, locker room floors, and swimming pools. Your risk of getting it may also increase by wearing tight-fitting, closed-toe shoes, or by having sweaty feet.
Symptoms of athlete’s foot include itching, stinging or burning sensations between the toes. You may also experience toenails that are discolored, thick, crumbly, or toenails that pull away from the nail bed.
Your podiatrist may diagnose athlete’s foot by detecting these symptoms or by doing a skin test to see if there is a fungal infection present. The most common exam used to detect Athlete’s foot is a skin lesion potassium hydroxide exam. To use this method, your doctor will scrape off a small area of the infected skin and place it into potassium hydroxide. The potassium hydroxide will destroy the normal cells and leave the fungal cells untouched so that they are visible under a microscope.
There are a variety of treatment options for athlete’s foot. Some medications are miconazole (Desenex), terbinafine (Lamisil AT), clotrimazole (Lotrimin AF), butenafine (Lotrimin Ultra), and tolnaftate (Tinactin). While these options may be able to treat your fungus, it is best that you consult with a podiatrist in order to see which treatment option may work best for you.
In some cases, Athlete’s foot may lead to complications. A severe complication would be a secondary bacterial infection which may cause your foot to become swollen, painful, and hot.
There are ways that you can prevent athlete’s foot. Washing your feet with soap and water each day and drying them thoroughly is an effective way to prevent infections. You also shouldn’t share socks, shoes, or towels with other people. It is crucial that you wear shower sandals in public showers, around swimming pools, and in other public places. Additionally, you should make sure you wear shoes that can breathe and change your socks when your feet become sweaty. If you suspect that you have Athlete’s foot, you should seek help from a podiatrist as soon as possible.
When Do I Need to See a Podiatrist?

Foot problems can signal underlying health issues that can worsen if ignored. For instance, neuropathy, resulting from nerve damage, can lead to numbness in the feet and make it hard to detect injuries. Conditions like diabetes frequently result in neuropathy, but a podiatrist is medically trained to offer treatments to manage symptoms. Changes in foot color can signal underlying issues like infections or poor circulation, and identifying and addressing these issues early is essential for effective treatment. Bunions, a deformity of the big toe, can cause discomfort and reduce mobility, but a podiatrist can recommend suitable footwear and a variety of treatment options to alleviate discomfort. Whether from high-impact exercises or wearing improper footwear, foot soreness should not be ignored. Podiatrists can prescribe custom orthotics to help alleviate pain and improve gait problems. Various musculoskeletal disorders can cause foot pain, and podiatrists can provide medication, foot padding, and other treatments to manage symptoms and improve mobility. If you have foot problems that interfere with daily activities, it is suggested that you schedule an appointment with a podiatrist.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
Symptoms of a Broken Foot

A broken foot often results from a sudden or traumatic injury and requires early recognition for appropriate treatment. While symptoms may overlap with less severe injuries like sprains, specific signs of a broken foot indicate a more serious issue needing immediate medical attention. Sensations of bones out of place or grinding within the foot may signal a break, warranting minimal movement to prevent further damage. Swelling, often accompanied by extreme pain, is common with a broken foot, persisting longer and more pronounced than a sprain. Bruising near the fracture site, spreading over time, indicates a broken foot, and requires evaluation from a podiatrist if persistent or worsening. Difficulty bearing weight on the foot, in addition to restricted movement and intense pain, suggests a broken bone. Immediate medical attention aids in accurate diagnosis and treatment planning. Seeking prompt evaluation from a podiatrist is imperative, and X-rays are essential for confirmation. Treatment typically involves immobilization with a splint or cast to support proper healing. If you suspect a broken bone in your foot, it is suggested that you make an emergency appointment with a podiatrist for an exam and diagnosis.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
Causes of Foot Pain in Seniors

Foot pain among older adults is a common issue, often caused by wearing improper footwear and physical changes in the feet as a result of aging. Wearing ill-fitting shoes, such as those that are too small, narrow, or high-heeled, can lead to discomfort and an increased risk of falls. Over time, the natural cushioning under the heel and ball of the foot decreases and arches become flatter, all of which can contribute to foot pain. Furthermore, as the joints in the feet stiffen and skin becomes drier, vulnerability to foot infections increases. Many underlying health conditions, including diabetes, arthritis, neuropathy, poor circulation, and obesity can add to foot problems in older adults. A podiatrist can help to determine the cause or causes of foot pain in seniors, and is followed by a suggested program of treatment. Options may include wearing proper footwear, prescribing foot exercises, and creating custom orthotic devices to reduce the foot pain. If you are experiencing foot problems associated with aging, it is suggested that you schedule an appointment with a podiatrist.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Renee Rodriquez, DPM from Foot Clinic of South Texas. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Brownsville, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.